Stage 2 pancreatic cancer represents a critical juncture in the progression of this often-deadly disease. It is classified into two subcategories: Stage 2A and Stage 2B. Understanding the differences between these stages, as well as the symptoms, causes, diagnostic processes, and treatment options, is crucial for anyone affected by this condition, whether directly or indirectly.
Stage 2 pancreatic cancer encompasses cancers that are considered locally advanced but have not yet metastasized extensively. In Stage 2A, the tumor exceeds 4 centimeters in size, which indicates a significant growth within the pancreas itself. Conversely, Stage 2B is characterized by the tumor being of any size but having spread to a maximum of three nearby lymph nodes. This occurs before the cancer can infiltrate more distant organs or tissues, making it a pivotal phase for intervention.
Symptoms: Recognizing the Signs
One of the perplexing aspects of pancreatic cancer is its often-late onset of symptoms. Many individuals may remain asymptomatic until the disease reaches Stage 2. When symptoms do manifest, they can include jaundice (yellowing of the skin and eyes), unintentional weight loss, fatigue, and abdominal pain, among others. These indicators may seem vague, allowing pancreatic cancer to evade early diagnosis, which complicates treatment challenges. Recognizing these signs early can potentially lead to earlier detection and better outcomes.
The root causes of pancreatic cancer remain largely elusive, but certain risk factors increase the likelihood of developing the disease. Notably, smoking is implicated in about 20% of Stage 2 cases, which situates tobacco use as a significant preventable factor. Other contributing elements include being over 55 years of age, obesity, genetic predispositions, and a history of the disease within a family. This combination of factors underscores the importance of lifestyle choices and genetic counseling in the fight against pancreatic malignancies.
Determining whether pancreatic cancer has advanced to Stage 2 necessitates a series of diagnostic tests administered by healthcare professionals. These can include imaging techniques like MRI, CT, or ultrasound scans, which visualize the tumor’s size and location. Positron emission tomography (PET) scans may also be utilized to pinpoint cancerous cells in the body. A biopsy, where tissue samples are checked for cancer cells, plays a crucial role alongside tumor marker tests that help in assessing the growth rate of the cancer. This comprehensive approach allows for an informed treatment pathway.
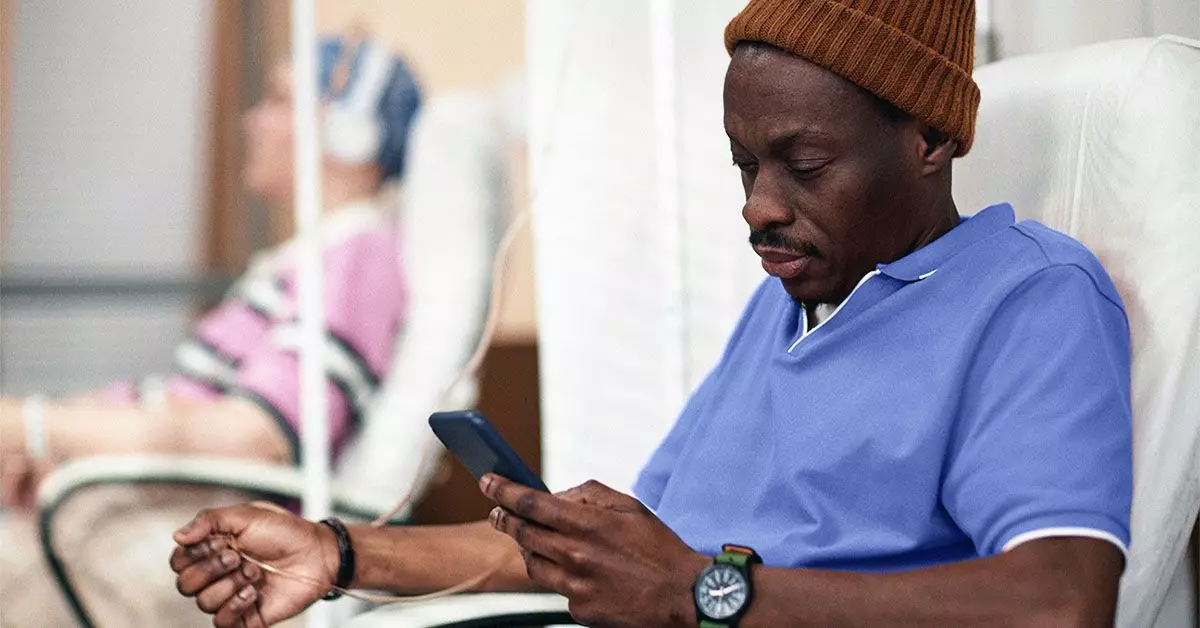
The treatment approach for Stage 2 pancreatic cancer typically involves a combination of surgery, chemotherapy, and potentially radiation therapy. For tumors categorized as resectable (able to be surgically removed), operations such as the Whipple procedure, total pancreatectomy, or distal pancreatectomy are considered to excise the tumor effectively. If the cancer is borderline resectable, preoperative chemotherapy may be recommended to shrink the tumor.
Additionally, adjuvant chemotherapy may be prescribed post-surgery to mitigate the risk of recurrence. Treatment plans are tailored to each individual, emphasizing factors such as tumor size, location, and lymph node involvement. An accurate prognosis often rests on the extent of disease spread and the individual’s overall health, highlighting the importance of personalized medical consultation.
Advancing to Stage 2 is a critical point in pancreatic cancer progression, but it does not guarantee a favorable outcome. The five-year survival rate for pancreatic cancer is distressingly low, typically ranging between 5% to 15%. This stark statistic underlines the importance of understanding the complex nature of the disease and the need to approach treatment with realism and determination.
While early detection and innovative treatments may improve chances, the experience of each patient varies significantly based on personal health factors and response to interventions. Ongoing dialogue with healthcare providers is essential for managing expectations and exploring all available treatment avenues.
Stage 2 pancreatic cancer highlights the urgent need for awareness regarding its symptoms, risk factors, diagnostic strategies, and treatment options. Each step taken, from recognizing early signs to undergoing appropriate medical evaluations, contributes to the broader fight against this formidable disease. Understanding and addressing pancreatic cancer together can spark hope for improved diagnosis, treatment, and patient outcomes. Each story shared helps to build a supportive community where knowledge empowers the fight against cancer.