Blood donation plays a critical role in saving lives, providing essential blood products for those in need. However, many donors may not be fully aware of the rigorous processes involved in ensuring the safety and efficacy of donated blood. Before a person donates, they undergo a detailed health assessment designed to evaluate their suitability for blood donation. This screening includes checks on vital signs such as pulse, blood pressure, and temperature, along with hemoglobin levels, which serve as indicators of a donor’s overall health. Hemoglobin, a crucial protein found in red blood cells responsible for oxygen transport, is a focal point in this assessment, as low levels can signal various health issues, including potential underlying conditions like leukemia.
While blood donation centers rigorously test for various infectious diseases and genetic markers, leukemia itself is not typically included in routine screening protocols. This oversight is significant, particularly given that leukemia may not present noticeable symptoms in its early stages. However, during the health assessment prior to donation, underlying health concerns may come to light. If a donor presents with low hemoglobin or signs of anemia, they are often ineligible to donate. More importantly, individuals with a prior diagnosis of leukemia are permanently disqualified from donating blood products. This precautionary measure is vital to protect both the donor and potential recipients from unsafe blood transfusions.
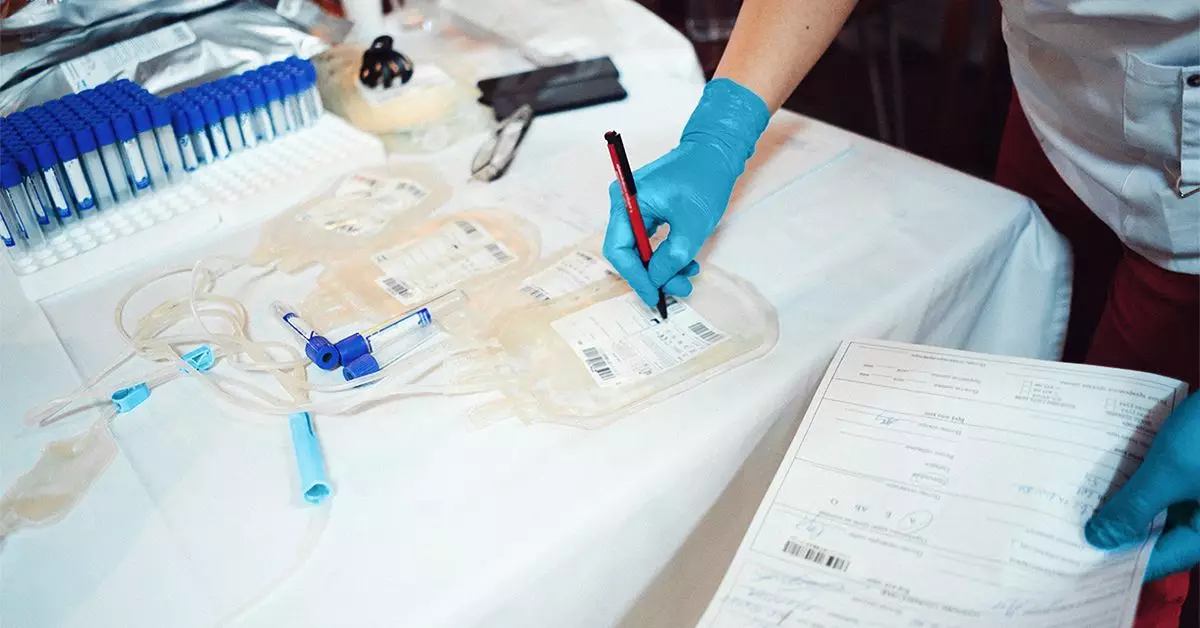
The American Red Cross and other blood donation organizations emphasize the importance of comprehensive blood screening following donation. These procedures involve various tests aimed at identifying the blood type and screening for certain infectious diseases, such as HIV, hepatitis, and syphilis. A lesser-known risk factor is the HTLV-1 virus, which can potentially lead to adult T-cell leukemia. Although incidents of ATL are rare, a positive result for HTLV-1 leads to the automatic disposal of the donation, alongside a notification to the donor. This demonstrates the commitment of blood donation centers to maintaining the highest safety standards.
An essential aspect of the blood donation process involves communication. If any abnormalities are detected in a donor’s blood, donation centers have protocols in place to reach out to the individual. This communication is critical as it encourages donors to follow up with healthcare professionals who can provide further testing and insight. Such proactive measures are vital not only for the donors’ peace of mind but also for their overall health management.
The relationship between blood donation and health conditions such as leukemia underscores the importance of awareness and transparency. For potential donors, understanding the screening process, the implications of their health status, and the potential risks associated with blood donation is essential. As communities engage in the lifesaving act of donating blood, they should remain informed and vigilant, ensuring individual and collective health remains a top priority in the noble pursuit of compassion and altruism through blood donation.